. 04/10/2024 4:08 PM
A Groundbreaking Medical Milestone
In a monumental achievement in the field of diabetes treatment, scientists have successfully reversed type 1 diabetes in a human for the first time using reprogrammed stem cell transplants. This medical breakthrough could potentially transform the way millions of people around the world live with type 1 diabetes, a condition once considered incurable. A 25-year-old woman from Tianjin, China, who had battled type 1 diabetes for over a decade, became the first person to produce her own insulin after receiving a transplant of reprogrammed stem cells derived from her own body.
The success of this procedure, documented in the prestigious scientific journal Cell, marks a significant advancement in regenerative medicine. The treatment offers hope for a cure for a condition that affects hundreds of millions globally. This article will explore the intricate details of the procedure, the implications of this medical advancement, and answer some key questions regarding its potential impact on the future of diabetes treatment.
.png1728041118.png)
Type 1 diabetes is an autoimmune disorder where the body’s immune system attacks and destroys insulin-producing beta cells in the pancreas. Without insulin, the body cannot regulate blood sugar levels, leading to severe complications like heart disease, nerve damage, and kidney failure. Patients with type 1 diabetes must rely on insulin injections to control their blood sugar levels, as their body is incapable of producing this vital hormone.
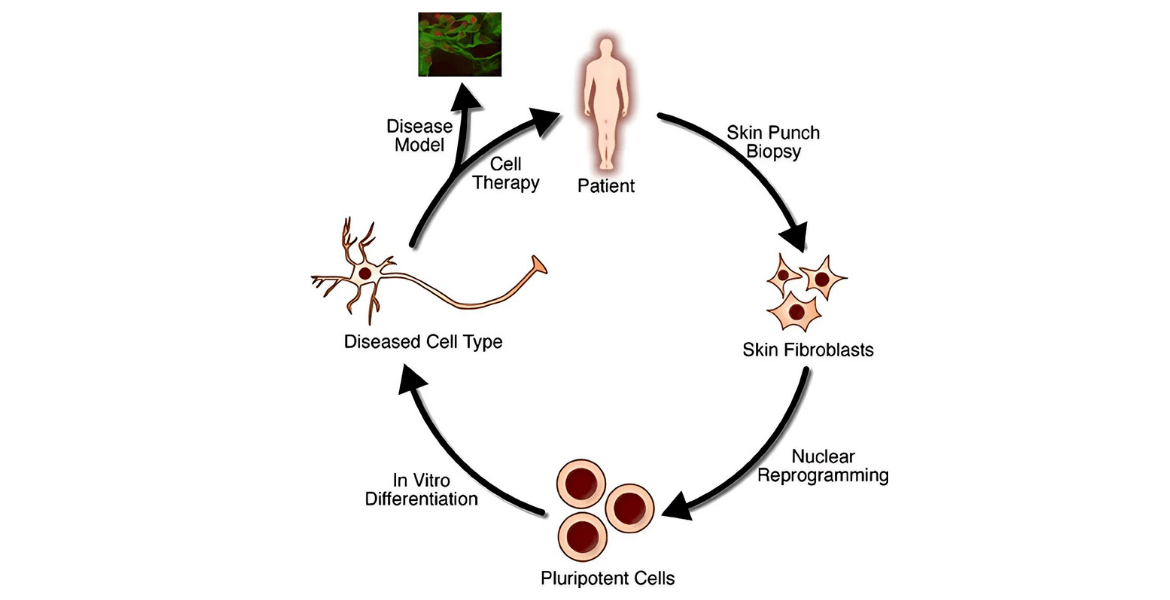
The groundbreaking procedure involved utilizing chemically induced pluripotent stem cells (CiPSCs). These are adult cells that have been reprogrammed into a pluripotent state, meaning they can develop into any cell type in the body, including insulin-producing beta cells. This method was first developed by Japanese scientist Shinya Yamanaka in the early 2000s, but the Chinese team, led by Dr. Deng Hongkui from Peking University, enhanced the technique by using small molecules instead of proteins to induce reprogramming, providing more precise control.
The cells were extracted from the patient’s adipose (fat) tissue, reprogrammed into CiPSCs, and then transformed into islet cells, which are responsible for producing insulin. These islet cells were injected into the patient’s abdominal muscles—a new site for islet transplants—allowing for easy monitoring and removal, if necessary. Traditional islet transplants are injected into the liver, but this method poses risks of inflammation and makes it difficult to observe the transplanted cells.
Less than three months after the stem cell transplant, the 25-year-old patient began producing her own insulin. This was the first time in over a decade that her body had naturally regulated its blood sugar. The clinical data revealed that 75 days post-transplantation, the patient achieved insulin independence, with her blood sugar levels stabilizing to within the target range for over 98% of the day.
Before the transplant, the patient had suffered from frequent spikes and drops in her blood sugar, alongside severe hypoglycemic episodes. However, after the treatment, her glycemic control stabilized, and her need for external insulin injections was eliminated. One year post-transplant, the patient’s condition remained stable, with no signs of transplant-related complications or rejection of the transplanted cells.
Islet transplants have long been considered a promising treatment for type 1 diabetes, but they are severely limited by the availability of donors. In traditional transplants, islet cells are taken from the pancreas of deceased donors and implanted into the liver of the recipient. This procedure is complicated by donor shortages and the need for immunosuppressant drugs to prevent rejection of the transplanted cells.
The use of stem cells circumvents both of these major challenges. Stem cells can be cultured indefinitely in the lab, providing a potentially limitless source of islet cells. Moreover, because the cells are derived from the patient’s own body, there is no risk of immune rejection, which eliminates the need for lifelong immunosuppressants.
This groundbreaking trial is not the only example of stem cell research pushing the boundaries of diabetes treatment. Earlier in 2024, a separate group of researchers in Shanghai successfully transplanted insulin-producing islet cells, derived from reprogrammed stem cells, into the liver of a 59-year-old man with type 2 diabetes. Like the woman from Tianjin, he too became insulin-independent within three months of the transplant.
While both studies represent significant progress, researchers caution that more clinical trials are necessary to ensure the long-term viability of these treatments. The Tianjin study’s success is a promising first step, but the researchers plan to extend the trial to another 10 or 20 participants in the coming year to gather more data.
Despite the success of this procedure, there are still hurdles to overcome before it can be widely available. One major challenge is scaling up the production of CiPSCs for widespread use. Creating personalized stem cell treatments is time-consuming and costly, which may limit accessibility in the near term.
Furthermore, while the patient in Tianjin was already on immunosuppressants due to a prior liver transplant, it remains to be seen how effective the CiPSCs will be in preventing immune rejection in patients who are not on such medications. Researchers are currently developing techniques to modify these cells to evade autoimmune attacks, a common problem in type 1 diabetes.
Several leading scientists and doctors have weighed in on this groundbreaking achievement. James Shapiro, a transplant surgeon from the University of Alberta, described the results as “stunning,” noting that the procedure has completely reversed diabetes in the patient. Daisuke Yabe, a diabetes researcher from Kyoto University, expressed optimism but emphasized the need for more clinical trials to determine if the results can be replicated in other patients.
Jay Skyler, an endocrinologist at the University of Miami, cautioned that it is too soon to declare the patient cured. He noted that the woman’s insulin production needs to be sustained for at least five years before such a conclusion can be drawn.
1. What makes this case unique in diabetes treatment?
This is the first time that a patient with type 1 diabetes has been treated using reprogrammed stem cells derived from her own body. The success of the procedure allowed the patient to produce insulin naturally, eliminating the need for insulin injections.
2. How does the stem cell transplant work?
The treatment involved reprogramming fat cells from the patient’s body into CiPSCs. These stem cells were then transformed into insulin-producing islet cells, which were transplanted into the patient’s abdominal muscles.
3. Why is this procedure significant?
This breakthrough offers hope for a cure for type 1 diabetes, a condition that affects millions of people worldwide. It eliminates the need for donor islets and immunosuppressant drugs, two major challenges in traditional islet transplants.
4. What are the potential risks of this treatment?
One potential risk is that the body may reject the transplanted cells. However, because the stem cells are derived from the patient’s own body, the risk of rejection is significantly lower than in traditional transplants. More clinical trials are needed to assess the long-term viability of the treatment.
5. Could this procedure work for other patients?
While the results from this case are promising, more studies are required to confirm whether this procedure can be replicated successfully in other patients. The researchers plan to expand the trial to include more participants in the near future.
6. What are the next steps in this research?
The team is planning to extend the clinical trials to 10 or 20 more patients. They are also working on developing CiPSC islet cells that can evade autoimmune attacks, which is a key issue for many people with type 1 diabetes.
The success of this stem cell transplant represents a significant leap forward in the treatment of type 1 diabetes. While more research is needed, the implications of this breakthrough could lead to a future where millions of people living with diabetes no longer have to rely on insulin injections. The next few years will be crucial in determining whether this groundbreaking procedure can truly transform diabetes care on a global scale.